Earlier this month, the Obama administration delayed implementing one component of the Affordable Care Act (ACA) – the provision that requires large employers to pay a penalty if they fail to offer health insurance coverage. The decision gives the federal government more time to clarify the rules and gives businesses more time to comply. A recent study by the Urban Institute assures us that it will not slow down the ACA’s goal to reduce the number of uninsured.
Let’s start with a little background. There are two “shared responsibility provisions” in the ACA, one for individuals and one for employers. They are often referred to as the individual and employer mandates.
 The individual mandate requires that nearly everyone have health insurance beginning January 1, 2014, or face a fine. The individual mandate creates an incentive for more people, including healthy people, to get insurance. It also creates an incentive for employers to offer insurance because there will be greater demand from their workers.
The individual mandate requires that nearly everyone have health insurance beginning January 1, 2014, or face a fine. The individual mandate creates an incentive for more people, including healthy people, to get insurance. It also creates an incentive for employers to offer insurance because there will be greater demand from their workers.
The employer mandate requires that large employers – those with 50 or more full-time equivalents (FTEs) – offer their full-time employees health insurance that meets certain standards. If they fail to do so, and any of their employees receive federal tax credits to purchase insurance on their own, the employer must pay a penalty. It’s this employer mandate and penalty that the federal government has delayed enforcing until 2015.
The employer penalty allows the federal government to recoup some of the public costs that result when employers don’t offer insurance. Many businesses already offer insurance to their employees because they understand the importance of a healthy workforce and know the value of insurance in attracting quality employees. The employer mandate asks larger businesses that fail to offer insurance to share the financial responsibility of providing tax credits to help their employees buy insurance on their own.
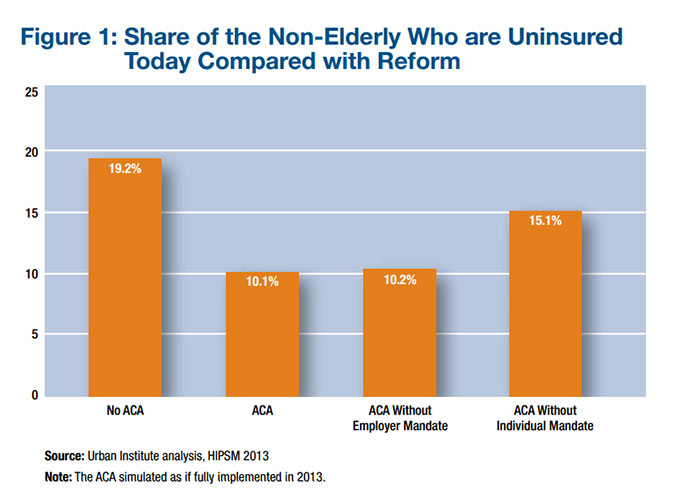
The Urban Institute study finds the decision to delay enforcement of the employer mandate will have little effect on increasing the number of people with health insurance. Even with the delay, if all other elements of the ACA are implemented, the share of people without insurance is predicted to fall from 19.2 percent to 10.2 percent. That’s a miniscule 0.1 percentage point higher than if the employer mandate was not delayed.
This should not come as a surprise. Many employers will continue to offer insurance for the same reasons they do now – it attracts good workers and keeps them productive. Other individuals will get insurance thanks to expanded eligibility for valued public health insurance opportunities, like Medicaid.
The greatest impact of delaying the employer mandate will be on the federal government, which will not collect a previously expected $3.7 billion in employer penalties. For the people the ACA is intended to help – the currently uninsured and underinsured – delaying the employer mandate will barely be a bump in the road.
-Christina Wessel